Arteriovenous Malformations: Challenges in Neurosurgical Treatment
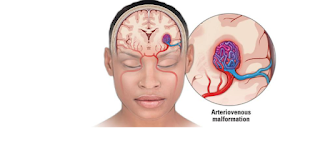
Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels in the brain or spinal cord that connect arteries directly to veins, bypassing the capillaries. These malformed blood vessels can disrupt normal blood flow and oxygen delivery to surrounding brain tissue. AVMs can present with a range of symptoms, including headaches, seizures, neurological deficits, and in severe cases, a hemorrhagic stroke due to vessel rupture.
When AVMs cause significant symptoms or complications, treatment is often necessary. Neurosurgical treatment options include surgery, radiosurgery, and endovascular embolization. Each of these methods comes with unique challenges, and the optimal treatment depends on factors such as the location, size, and depth of the AVM, as well as the patient’s age, health, and other risk factors.
This article explores the challenges in the neurosurgical treatment of AVMs, including the complexity of surgical planning, risks, and decision-making processes involved.
Challenges in Neurosurgical Treatment of AVMs
Location and Accessibility:
- Intracranial AVMs: AVMs located deep within the brain or near critical areas such as the brainstem or eloquent areas (e.g., areas responsible for motor function, speech, or vision) present significant surgical challenges. These regions are difficult to access, and surgical intervention carries a risk of damaging vital brain structures.
- Spinal AVMs: AVMs in the spinal cord are also challenging to treat. Surgical access to the spinal cord can be complex, and there are risks of damaging the spinal cord itself during surgery.
- Venous Drainage: AVMs often have a complex venous drainage system. In some cases, the veins that drain the AVM can be large and difficult to remove or embolize without risking damage to surrounding tissue, potentially causing neurological deficits.
Size and Shape of the AVM:
- Large AVMs: Larger AVMs have a higher risk of rupture and can be more difficult to remove completely. A larger size may also mean that they have more extensive blood vessels that are harder to access surgically.
- Multiple Feeding Vessels: AVMs may have several arteries feeding them, and it can be difficult to identify and occlude all of these vessels during surgery. Incomplete removal of the AVM can result in recurrence or persistent symptoms.
- Nidus Shape: The shape of the AVM’s nidus (the tangle of vessels) can affect its surgical accessibility. Complex, irregular-shaped AVMs may be difficult to reach, especially if they are located near critical structures or deep within the brain.
Risk of Bleeding and Hemorrhage:
- Intraoperative Bleeding: AVMs are often surrounded by fragile blood vessels that are prone to bleeding. Surgical resection of an AVM requires careful handling to avoid accidental rupture of these vessels, which can lead to massive bleeding and potentially catastrophic consequences.
- Postoperative Hemorrhage: Even after surgery, there is a risk of bleeding, either from the residual AVM or from newly disrupted blood vessels. Postoperative bleeding can lead to brain swelling, increased intracranial pressure, and worsening neurological deficits.
- Recurrent Bleeding: In cases where AVMs are not fully removed or treated, recurrent bleeding can occur. This is especially a concern in patients with large AVMs or those that are difficult to access.
Functional Outcome and Risks to Neurological Function:
- Risk to Nearby Brain Tissue: Surgical resection of AVMs, especially those in or near eloquent areas of the brain, carries the risk of damage to vital functions such as speech, motor control, and sensory processing. Even if the AVM is completely removed, there is a possibility of post-surgical neurological deficits if healthy brain tissue is inadvertently harmed.
- Cognitive and Motor Function: Surgery can impact cognitive abilities, movement, and coordination, depending on the location of the AVM and the success of the resection. Rehabilitation may be necessary to regain lost functions.
- Psychological Impact: The potential for neurological impairment can also have psychological and emotional consequences for patients, as the loss of independence or cognitive abilities can lead to depression and anxiety.
Multidisciplinary Approach:
- Treating an AVM often requires a multidisciplinary team approach. Neurosurgeons, interventional radiologists, neurologists, and other specialists need to collaborate to determine the most appropriate treatment for each patient. This is especially important for complex cases where a combination of surgical, endovascular, and radiosurgical approaches may be required.
Treatment Options and Their Challenges
Surgical Resection:
- Procedure: Surgical resection is considered the gold standard for AVM treatment when the AVM is accessible and the risk of bleeding can be managed. The goal is to remove the entire AVM and restore normal blood flow to the brain.
- Challenges: The primary challenges include the complexity of the AVM’s location, size, and blood supply, as well as the risk of intraoperative bleeding and potential damage to surrounding brain structures.
- Outcomes: Successful resection can cure the AVM, eliminating the risk of rupture, but the risk of postoperative deficits is a significant consideration, particularly in eloquent brain areas.
Endovascular Embolization:
- Procedure: Endovascular embolization involves the insertion of a catheter into the blood vessels, typically via the groin, and the injection of embolic agents to block the blood flow to the AVM.
- Challenges: Endovascular embolization may not be effective for all AVMs, particularly those that have large or multiple feeding arteries. Incomplete embolization can lead to recurrence or persistent symptoms. The procedure also requires skilled interventional radiologists to navigate the vascular anatomy.
- Outcomes: Embolization is often used as a pre-surgical procedure to reduce the size of the AVM or to facilitate complete resection. In some cases, embolization may be the primary treatment for small or accessible AVMs.
Radiosurgery (Gamma Knife or Linear Accelerator):
- Procedure: Radiosurgery involves delivering high doses of focused radiation to the AVM, which gradually causes the blood vessels within the AVM to clot and close off.
- Challenges: Radiosurgery is typically used for smaller AVMs or those in locations that are difficult to reach surgically. The primary challenge is that the AVM does not close immediately after treatment. It can take months or even years for the AVM to fully occlude, leaving a window of time where there is still a risk of bleeding.
- Outcomes: Radiosurgery is generally less invasive and carries lower risks compared to surgery. However, it may not be effective for large or complex AVMs, and the risk of rupture before the AVM closes off is a concern.
Challenges in Decision-Making:
Deciding the best course of action for AVM treatment requires careful consideration of multiple factors:
- Size and Location: The size and location of the AVM dictate which treatment is most appropriate. Large or deep AVMs may require a combination of approaches, such as embolization followed by surgery or radiosurgery.
- Age and Health Status: The patient’s age and overall health are critical factors in determining whether a more invasive surgical approach or a less invasive option like embolization or radiosurgery is preferred.
- Risk of Bleeding: The risk of an AVM rupture, especially if it is symptomatic, often guides treatment decisions. Ruptured AVMs typically require immediate intervention, and timing is critical in preventing further complications.
- Long-Term Follow-Up: AVM patients require careful follow-up care to monitor for recurrence or complications following treatment. Long-term imaging (e.g., MRI or angiography) is necessary to assess the success of the treatment and detect any residual AVM or new issues.
Conclusion
The treatment of arteriovenous malformations (AVMs) presents significant challenges in neurosurgery due to the complexity of the condition, the diverse treatment options, and the risks involved in each approach. Neurosurgeons must carefully evaluate the AVM’s location, size, and associated risks before deciding on the most appropriate treatment plan. Although surgical resection remains a highly effective option for certain AVMs, endovascular embolization and radiosurgery offer minimally invasive alternatives for patients who are not suitable candidates for traditional surgery. A personalized, multidisciplinary approach is essential to achieving the best possible outcomes while minimizing risks to the patient’s neurological function and overall health.
Would you like more information on any of these treatment methods or their specific indications?