Brain Metastases in Lung Cancer: The Neurosurgical Approach
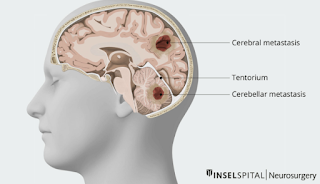
Brain metastases are a common complication of lung cancer, particularly in non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). These secondary brain tumors significantly affect prognosis and quality of life. Neurosurgery plays a pivotal role in managing brain metastases, particularly for patients with solitary lesions or symptomatic tumors, as part of a multidisciplinary treatment approach.
Overview of Brain Metastases in Lung Cancer
- Incidence: Lung cancer is the leading cause of brain metastases, occurring in up to 30–50% of patients during their disease course.
- Pathophysiology: Tumor cells from the lung travel via the bloodstream and colonize the brain, often forming well-circumscribed lesions.
- Symptoms:
- Neurological deficits: Weakness, numbness, or difficulty speaking.
- Seizures: Common in patients with cortical involvement.
- Increased intracranial pressure: Headaches, nausea, and visual disturbances.
Role of Neurosurgery in Management
Surgery is a cornerstone for managing brain metastases in select lung cancer patients. The goals of neurosurgical intervention include:
- Tumor Removal:
- Reduces mass effect and relieves symptoms like headaches and neurological impairments.
- Improves local tumor control, particularly for solitary or dominant lesions.
- Diagnosis:
- Provides tissue for histopathological analysis to confirm metastasis and identify biomarkers for targeted therapy.
- Prolonged Survival:
- In appropriately selected patients, surgery can extend survival when combined with systemic and local therapies.
Indications for Surgery
Surgery is typically recommended for:
- Solitary Brain Metastases:
- Particularly in patients with controlled systemic disease and good performance status (e.g., Karnofsky Performance Score >70).
- Symptomatic Lesions:
- Tumors causing significant mass effect, edema, or life-threatening conditions such as brainstem compression.
- Diagnostic Uncertainty:
- When imaging is inconclusive, and a biopsy is needed to guide treatment.Advances in Neurosurgical Techniques
- Preoperative Imaging:
- MRI with contrast and functional imaging helps delineate tumor boundaries and map critical brain areas.
- Neuronavigation:
- Real-time image-guidance systems enable precise targeting and minimize damage to healthy tissue.
- Intraoperative Monitoring:
- Functional monitoring during awake craniotomy protects critical brain regions, such as those controlling speech or movement.
- Minimally Invasive Approaches:
- Endoscopic-assisted resection or stereotactic biopsy for deep-seated or inaccessible tumors.
- Intraoperative MRI/CT:
- Provides real-time updates to ensure maximal tumor removal while avoiding critical areas.
Combined Therapies for Optimal Outcomes
Neurosurgery is often integrated with other treatments for comprehensive care:
- Stereotactic Radiosurgery (SRS):
- Precise, high-dose radiation to the surgical cavity or unresected metastases.
- Whole-Brain Radiation Therapy (WBRT):
- Used for multiple metastases but associated with cognitive side effects, limiting its use in modern practice.
- Targeted Therapy:
- EGFR inhibitors (e.g., osimertinib) and ALK inhibitors (e.g., alectinib) are effective in molecularly defined subtypes of lung cancer with brain involvement.
- Immunotherapy:
- Checkpoint inhibitors like pembrolizumab have shown promise in systemic and intracranial disease control.
Risks and Challenges
- Recurrence:
- High likelihood of new or recurrent metastases due to the ongoing systemic nature of lung cancer.
- Complications:
- Risks include infection, bleeding, or neurological deficits post-surgery.
- Patient Selection:
- Surgery is generally reserved for patients with a favorable prognosis, as aggressive interventions may not benefit those with extensive systemic disease.
Outcomes and Prognosis
- Improved Survival:
- Median survival for patients with resected solitary brain metastases is 12–18 months when combined with effective systemic therapy.
- Symptom Relief:
- Surgery effectively alleviates mass effect and neurological symptoms in most cases.
- Prognostic Factors:
- Controlled systemic disease, good performance status, and absence of extracranial metastases predict better outcomes.
Emerging Frontiers
- Molecular and Genetic Insights:
- Liquid biopsies and next-generation sequencing help tailor treatments to individual tumors.
- Minimally Invasive Neurosurgery:
- Techniques like Laser Interstitial Thermal Therapy (LITT) are being explored for hard-to-reach metastases.
- Artificial Intelligence:
- AI-assisted imaging and predictive models are improving surgical planning and outcome assessments.
Conclusion
Neurosurgery plays a critical role in managing brain metastases from lung cancer, particularly for patients with solitary or symptomatic lesions. Advances in surgical techniques and integration with systemic therapies have improved outcomes and quality of life. A multidisciplinary approach remains essential to optimize care, balancing aggressive local treatment with systemic disease management.
Would you like to explore specific surgical techniques, systemic therapies, or patient selection criteria in more detail?