Understanding Pediatric Hydrocephalus and Its Surgical Treatment
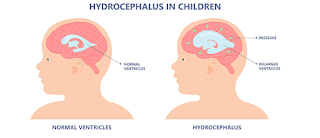
Hydrocephalus is a neurological condition characterized by an abnormal accumulation of cerebrospinal fluid (CSF) within the ventricles (cavities) of the brain. This buildup of fluid can lead to increased pressure within the skull, which may result in damage to brain tissues and disrupt normal brain function. In pediatric patients, hydrocephalus can be a congenital (present at birth) or acquired condition, and it often requires surgical intervention to manage the increased pressure and prevent long-term developmental issues.
Types of Pediatric Hydrocephalus
- Congenital Hydrocephalus:
- Present at birth, often caused by genetic factors or issues during fetal development.
- Common causes include:
- Aqueductal Stenosis: Narrowing of the aqueduct (the duct that allows CSF to flow between the brain's ventricles).
- Chiari Malformation: A condition where brain tissue extends into the spinal canal.
- Spina Bifida: A birth defect in which the spinal cord does not develop properly.
- Intraventricular Hemorrhage: Bleeding within the ventricles, often seen in premature infants.
- Acquired Hydrocephalus:
- Develops after birth due to injury, infection, or disease.
- Causes include:
- Brain tumors that block CSF flow.
- Infections such as meningitis or encephalitis.
- Traumatic brain injury that leads to CSF blockage or bleeding.
- Cysts or other structural brain abnormalities.
Symptoms of Pediatric Hydrocephalus
The symptoms of hydrocephalus can vary based on the child's age, the severity of the condition, and whether the hydrocephalus is congenital or acquired. Common symptoms include:
Infants:
- Rapid head enlargement (due to the soft skull bones).
- Bulging fontanel (the "soft spot" on the baby’s head).
- Vomiting.
- Irritability or poor feeding.
- Abnormal eye movements (sunsetting eyes).
- Seizures.
- Delayed development or failure to meet milestones.
Older Children:
- Headache.
- Nausea and vomiting.
- Difficulty with balance or coordination.
- Visual problems, such as blurred or double vision.
- Cognitive delays or learning difficulties.
- Abnormal gait or difficulty walking.
- Urinary incontinence or difficulty with bladder control.
Diagnosis of Pediatric Hydrocephalus
Clinical Evaluation:
- A pediatric neurologist or neurosurgeon will perform a thorough clinical evaluation, considering symptoms, medical history, and a physical examination.
- Measurement of head circumference is often used in infants to track any unusual growth.
Imaging Studies:
- MRI (Magnetic Resonance Imaging): Provides detailed images of the brain and is the most common and accurate diagnostic tool for hydrocephalus.
- CT Scan (Computed Tomography): Used when MRI is not available or practical, especially in emergency situations.
- Ultrasound: Used in infants, especially those with an open fontanel, as it can provide images of the ventricles.
Intracranial Pressure Monitoring:
- In some cases, monitoring of the CSF pressure may be done to determine the severity of the condition.
Surgical Treatment of Pediatric Hydrocephalus
Surgical intervention is typically required to treat hydrocephalus and alleviate the increased pressure on the brain. The two main surgical options are:
Ventriculoperitoneal (VP) Shunt Placement:
- Procedure: A VP shunt is the most common surgical treatment for hydrocephalus. The shunt consists of a tube placed in one of the brain’s ventricles (where CSF accumulates), with a valve to regulate the flow of fluid. The tube is tunneled under the skin and connected to the peritoneal cavity (abdominal space) where excess CSF is absorbed.
- Goal: To divert the excess fluid from the brain and regulate the pressure.
- Post-Surgery Care: The child will typically stay in the hospital for a few days for observation. The shunt will require lifelong monitoring, and periodic follow-up visits are needed to check for any complications, such as infection or blockage.
- Complications: Common issues include shunt infection, blockage, or malfunction. Over time, the shunt may need to be adjusted or replaced as the child grows.
Endoscopic Third Ventriculostomy (ETV):
- Procedure: In certain cases of hydrocephalus, especially when caused by obstruction in the brain's ventricular system (such as aqueductal stenosis), an endoscopic third ventriculostomy may be performed. During this procedure, the surgeon uses a small camera (endoscope) to create a hole in the floor of the third ventricle, allowing CSF to flow more freely, bypassing the blockage.
- Goal: To create an alternative pathway for CSF drainage within the brain, thus avoiding the need for a shunt.
- Post-Surgery Care: Children undergoing ETV will typically stay in the hospital for observation for a few days. Follow-up imaging will be required to ensure proper CSF flow.
- Complications: While this procedure avoids the need for a shunt, there are still risks, including failure of the ventriculostomy, infection, and bleeding.
Shunt vs. ETV:
- Shunt placement remains the more commonly used method, but ETV is an option for specific cases, especially when the blockage is located in certain areas of the brain. The decision between these two procedures depends on factors such as the cause of hydrocephalus, age, and overall health of the child.
Post-Surgical Care and Recovery
Monitoring:
- After surgery, the child will be closely monitored for signs of infection, bleeding, or shunt malfunction.
- Follow-up visits are necessary to assess growth, development, and any complications related to the shunt or procedure.
Rehabilitation:
- Depending on the severity of the hydrocephalus, the child may need physical therapy, occupational therapy, or developmental support to address any delays in motor skills, cognition, or speech.
Long-Term Care:
- Lifelong follow-up care is required for children with shunts to ensure that the device continues to function properly and to address any issues that may arise, such as infections, blockages, or growth-related adjustments.
Prognosis and Outcomes
- With Treatment:
- Surgical treatment, particularly with VP shunt placement, can significantly improve the quality of life for children with hydrocephalus. Most children experience a reduction in symptoms and can lead a relatively normal life, though some may still face challenges with cognitive, motor, or sensory functions depending on the severity of the hydrocephalus and the timing of treatment.
- Without Treatment:
- If left untreated, hydrocephalus can lead to brain damage, developmental delays, and potentially life-threatening complications due to increased intracranial pressure.
Conclusion
Pediatric hydrocephalus is a serious condition that can lead to significant neurological issues if not treated promptly. Fortunately, with timely diagnosis and surgical intervention, the majority of children with hydrocephalus can lead functional and productive lives. Advances in surgical techniques, such as VP shunt placement and endoscopic third ventriculostomy, have dramatically improved outcomes for children with this condition. Regular monitoring and post-surgical care are essential for ensuring long-term success and preventing complications.
Would you like more information on specific aspects of hydrocephalus treatment or patient management?